The Significance of Childhood Neurosis for Adult Mental Health: A Follow-Up Study
by
Sherwood Waldron, Jr., M.D.
-
-
-
-
- Introduction
- Method
- Results
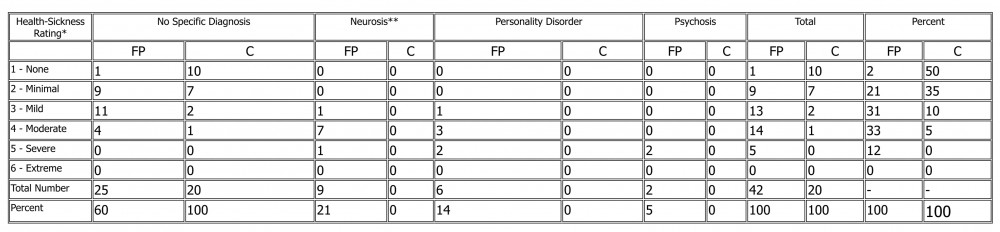
- Table 1: Health Sickness Ratings and Diagnosis at Follow-Up of 42 Former Patients (FP) and 20 Control Subjects (C)
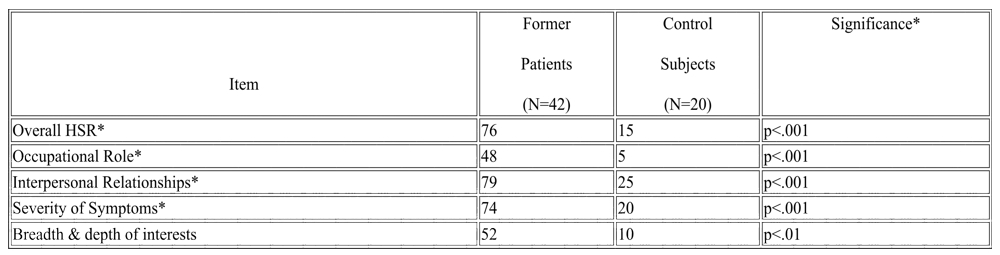
- TABLE 2: Percent of Former Patients and Control Subjects with More than Minimal Impairment of the Health-Sickness Rating Scale and Subscales
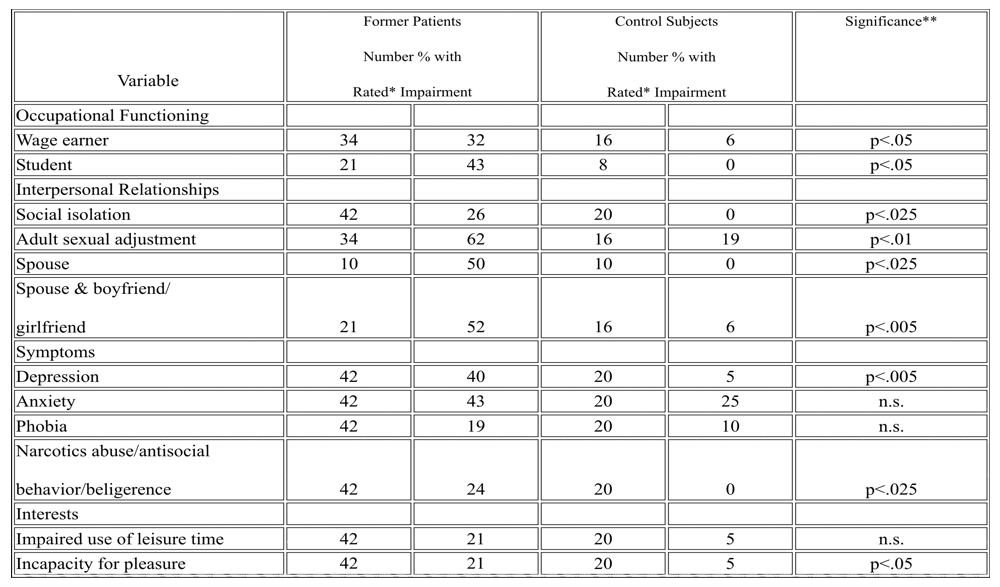
- TABLE 3: Percent of Former Patients and Control Subjects with More Than Minimal Impairment on Various CAPPS Ratings
- Discussion
- Conclusion
-
-
-
The author compared the mental health of 42 young adults who had suffered from a neurosis in childhood with that of 20 control subjects. Various aspects of functioning were clinically assessed using the Current and Past Psychotherapy Scales and the Health-Sickness Rating Scale. More than 75% of the former patients were at least mildly ill at follow-up, compared with only 15% of the control group. Intergroup differences in diagnosis and symptoms are described. The findings establish the fact that neurotic children require much more effective treatment than they have traditionally received in order to attain a good prognosis for adult mental health.
Introduction
Neurotic children may be referred for treatment because the presenting symptom itself is distressing, but more commonly treatment is considered on the basis of concern about the child’s future development. Because of a lack of adequate follow-up studies, we do not know for certain whether neurotic children have unfavorable long-term prognosis. Even the demonstration of short-term improvement with treatment ((1)) does not tell us whether such improvement predicts ultimate adult mental health, and there is reason to think that it does not ((2)).
The few long-term studies available ((3) (4)) suffer from deficiencies in design because they lack either a clinical evaluation of the patients of a control group. It is too hazardous to compare their findings with those of the epidemiological studies of psychiatric disturbance in the general population (e.g.(5) (6)) because the latter generally use a questionnaire-interview approach by nonprofessionals that may result in misleading conclusions when compared to the results of assessment by clinicians ((7)).
Several long term follow-up studies of children suffering from various specific neurotic symptoms ((8) (9) (10) (11) (12) (13)) have suggested the importance of these difficulties to adult mental health. I thought that a long-term follow-up study of neurotic children in general would be more interesting of we studied one of these subgroups as well. I chose children with school phobia because of the evidence that impairment continued into adolescence ((14)), while the symptom itself tends to remit during childhood with most short-term therapies. Therefore, extensive psychotherapy for this condition would ordinarily be indicated only if the long-term prognosis were unfavorable.
For two reasons, I selected the control group from children who were in the same elementary school class as each of our former patients. This sample would presumably reflect the normal expectable outcome for an unselected population, with the omission only of those children too disturbed or damaged to maintain attendance at an ordinary school. In addition, the selection method would serve as an effective control for age, sex, and social class.
We wanted to use a clinical appraisal of these young adults because of the tenuous relationship between indirect measures of mental health and clinical findings. Clinical assessment itself has often been found unreliable ((15) (16) (17)). Fortunately, two instruments have been developed, based on clinical appraisal, which have shown excellent reliability: The Menninger Clinic’s Health-Sickness Rating (HSR) Scale ((18) (19)), in which ratings are anchored to case descriptions, and the Current and past psychopathology Scales (CAPPS), a semi-structured clinical interview with rating scales developed by Endicott and Spitzer at Columbia University ((20)). These two instruments made possible a follow-up that would be both clinically meaningful and reliable.
Our research group independently assessed the clinical status of the children and their families when they were seen in out clinic in order to provide baseline values that sould be compared with outcomes and to clarify the syndrome or syndromes of school phobia. This systematic study has already been reported ((21)). (TOP)
Method
Subjects
A child psychiatrist screened the charts of all patients under 13 who were first evaluated at our clinic between 1955 and 1962 (N=627). Using the classification of psychopathological disorders in childhood of the Group for the Advancement of Psychiatry ((22)), we could differentiate between those children who suffered fro neurotic disorders or other milder conditions (e.g., reactive disorders or developmental disturbances) and the sicker children. Those who had experienced a school phobia were identified from among the neurotic group. Criteria of classification were first refined in a pilot series of charts, resulting in excellent interrater reliability.
Two-thirds of the over 600 children were considered sicker than neurotic and were excluded from further study. Forty-five of the 203 neurotic children were identified as having had school phobia. We drew up a panal of 35 subjects from the group with school phobia; this was the maximum number that we could study. We then matched one other neurotic child to each of these children with school phobia on the basis of sex, age at referral, and year of referral to the clinic. We selected our control subjects from the class that each child with school phobia was attending when the phobia first appeared; from each class we selected the child whose surname alphabetically followed that of the phobic child.
Procedures for locating the subjects were similar to those described by others ((23) (24)). Considerable persistence and ingenuity were required. Introductory letters were followed by a home visit unless the subject refused. Thus we visited the homes of nonresponders. The home visits were made as far as 200 miles from New York.
Primary Follow-Up Instruments
The semistructured clinical interview (the CAPPA) is of sufficient flexibility to permit the interviewer to explore areas of particular clinical significance as they emerge during the interview. The assessment includes various scales of symptomatology as well as leasurements of sexual and interpersonal relationships and functioning in the roles of spouse, parent, housewife, student, employee. We also added a few other individual scales of particular interest to us. Summary scales have been previously derived by factor analyses of the more than 170 CAPPS scales. A computer program has also been developed which produces reliable and valid psychiatric diagnoses when applied to these scale scores of each individual ((25)).
Most of the CAPPS scales use a 6-point rating ranging from “none” through “minimal,” “mild,” “moderate,” and “severe” to “extreme” on each dimension rated. We were particularly interested in the overall rating of severity of illness. There is a 6-point severity of illness scles of the CAPPS, which we coordinated with the 100-point HSR scale by achieving a consensus among 3 clinicians as to what points on the 100-point scale corresponded to the 6 degrees of severity of illness specified above. Each time we rated an individual for severity of illness on the CAPPS, we used the case descriptions provided with the HSR scale, gave a rating on the 100-point HSR scale, then converted it to the corresponding score for the severity of illness expressed in the 6-point scale (see footnote to table 1 for score conversions). We developed 4 subscales of this overall health-sickness rating, reflecting different aspects of mental health and based upon the 7 subscales originally developed at the Menninger Clinic.
Follow-Up Interviews
I concluded most of the interviews; the rest were done by another child psychiatrist. All of the interviews were tape recorded. Each of us was first trained and evaluated for reliability. Subsequently, ongoing reliability was monitored by independent ratings of an unselected sample of the tape recordings of interviews. Reliability was excellent for the various scales; for example, the most important judgment, the HSR score, showed an interclass correlation coefficient of .87 between the two raters. Neither interviewer had any knowledge of the old records or of the classification of the subject at the time of the interview, except as the subject revealed it himself in the course of the interview. (TOP)
Results
We were able to locate 91% of our 105 subjects, of whom two-thirds agreed to be interviewed. We saw 24 phobic subjects, 18 subjects with other neuroses, and 20 controls. Fifty-eight percent of the follow-up group were men. Most subjects were of middle- to lower- class origin. The subjects averaged 22 years old at follow-up; fewer than 5% were younger than 18.
The interviews lasted an average of 3 � hours. The interviews were so lengthy because we encouraged the subjects to discuss their life story in their own way. The interviewer then pursued pertinent lines of inquiry as in a regular initial psychiatric interview. Visiting homes in the absence of a response was important to our success, since one-third of those interviewed had not answered our letters (comparison of responders and nonresponders showed negligible mean differences in HSR scores).
We could compare the subjects who were interviewed with those who were not because we had extensive ratings of clinical aspects of the parents and families of virtually all of the former patients themselves as children. There were negligible differences between the 2 groups og subjects on all ratings from childhood. (See reference 21 for descriptions of the dimensions rated.) This finding reassures us that the 40% of our 105 subjects who were not seen in the follow-up were probably not very different from those who were seen.
Former Patients
When we compared those persons who had had a school phobia with those who had had other neuroses, we found that the phobic subjects 1) seemed more dependent (29% versus 6%), 2) had a greater tendency to somatize (42% versus 11%), and 3) had had more difficulty completing their secondary school education (25% versus 6%). Aside from these 3 findings, the goups were not distinguishable on our multiple leasures. These measures included a number of factors postulated in the literature as typical of school phobics in later years, such as leading lives more centered around the home of origin, tending to avoid new situations, and being more inhibited in the expression of aggression ((26)). Both groups of former patients were more inclined toward these behaviors than the control subjects were. Because there were so few differences between the 2 groups of former patients as a whole with the control group for the remainder of our analysis.
Diagnoses and Health-Sickness Ratings
The school-phobic patients did not differ as a whole from the other neurotic patients in distribution of diagnosis or degree of illness at follow-up. However, there were striking differences in these areas between the former patients as a whole and the control group.
Table 1
Health Sickness Ratings and Diagnosis at Follow-Up of 42 Former Patients (FP) and 20 Control Subjects (C)
* HSR scores on the 6-point scale correspond to the original 100-point scale as follows: 1=86-100, 2=76-85, 3=66-75, 4=51-65, 5=26-50, 6=0-25.
** The numbers for the neurosis have been corrected for computer overdiagnosis of phobic neurosis when the clinical picture did not warrant this specific diagnosis.
We found that 40% of the former patients, but none of the controls, received specific diagnoses from the computer program (p<.01, chi square analysis). Twenty-one percent of the former patients were diagnosed as having specific neurosis, (Four suffered from depressive neurosis; 2 from hysterical neurosis, conversion type; 1 from phobic neurosis; 1 from anxiety neurosis; and 1 from obsessive-compulsion neurosis.) 14% as having a personality disorder including drug dependence, and 5% as being psychotic, although neither of these 2 patients had ever been hospitalized. Thus we found a wide range of psychopathology in the former patients.
The HSR scales showed an even more striking difference between the former patients and the controls: more than 75% of the former patients were at least mildly ill, compared to only 15% of the controls (p=.001).
Since diagnoses were derived from computer analysis of the scores on specific variables, whereas the level of illness was a global rating by the interviewer, it is interesting to examine the relationship between the two. There were no specific diagnoses for those who were not ill or minimally ill, whereas close to half of those who were mildly to moderately ill received a specific diagnosis. The author, who is psychoanalytically trained, reviewed the cases of patients who were found to be ill but not diagnoses. All of them appeared to fit into the category of character disorders in the psychoanalytic sense ((27) ), although they were not suitable for diagnosis from DSM-II ((28) ).
The relationship between the nature and degree of illness of the 2 groups can be summarized as follows: 64% of the former patients were mildly to moderately ill, predominantly with a neurosis or character disorder, while another 12% were severely ill, predominantly with a personality disorder or psychosis. In contrast, only 15% of the control subjects were mildly to moderately ill, all with character disorders. None of the controls was more severely ill.
We were also interested in which of the different aspects of mental health was impaired. The data in table 2 demonstrate that the former patients were quite impaired in severity of their symptoms and in their interpersonal relationships and less impaired occupationally and in breadth of their interests. In all aspects they were substantially less healthy than the control subjects.
Individual CAPPS Variables
The clinical significance of the subscale differences between the two groups can be understood by examining specific clinical differences between them.
TABLE 2
Percent of Former Patients and Control Subjects with More than Minimal Impairment of the Health-Sickness Rating Scale and Subscales
* Significance was determined be analysis of variance over entire 6-point range (Student’s t test).
TABLE 3
Percent of Former Patients and Control Subjects with More Than Minimal Impairment on Various CAPPS Ratings
* Not all patients qualified for a rating on each of these variables.
** One-tailed chi-square analysis was used since the overall trend had been established.
The former patients showed greater difficulty than the controls in functioning as wage earners and as students, with about one-third being impaired. However, the differences between the 2 groups were not so great as in some other areas.
Disturbances in interpersonal relationships were extensive. More than one-fourth of the former patients were more than minimally socially isolated, compared to none of the controls; almost two-thirds had substantial problems in adult sexual adjustment, compared to only one-fifth of the controls. Because many of the subjects were just entering adulthood and therefore would not usually have married yet, we added an assessment of functioning as boyfriend or girlfriend to that of a spouse if the relationship seemed enduring and serious. If we examine spouses and boyfriends and girlfriends together, we find that only 50% of the former patients had such a relationship, compared to 80% of the controls (p=.025). Of the former patients who did have such a relationship, 52% of them were at least mildly impaired, compared to only 6% of the controls.
There were various symptomatic differences between the two groups. Nearly half of the former patients suffered from at least mild depression, compared with only 1 of the control subjects. They also had suffered more from anxiety and phobias than the controls, but the differences were not statistically significant. Almost one-fourth of the former patients showed more than a minimal degree of narcotics abuse and/or antisocial behavior and/or belligerence, compared with none of the controls. There were other symptomatic manifestations that were present in small numbers of the former patients; 2 patients had a history of homosexual acts and 1 patient had a perversion. More of the former patients also showed impaired use of lesiure time and incapacity for pleasurable activities. In all, there were many ways in which the former patients appeared to be more impaired than the control group (We might not have discovered the actual differences between the former patients and controls if we had assessed them during adolescence instead of young adulthood. Our retrospective assessment of functioning in adolescence showed only small differences in the quality of adolescent friendships, sexual adjustment, and academic performance. A substantial number of the control subjects, as well as the former patients, showed malfunction.).
Relationships Between the Various Measures
The differences between the former patients and the control subjects on individual variables were reflected in significant differences between the 2 groups on the relevant summary scales. The set of findings bears out the significant differences found in subscales of the HSR (See table 2) and adds a partly independent confirmation to the validity of our principal findings. This is because the summary scale scores are founded upon the individual variables, which are usually much more concrete and specific than the HSR subscales, leaving less latitude for rater bias. Intercorrelations between the HSR subscales and summary scales demonstrated the same relatively high degree of relationship between different aspects of mental health as had been previously demonstrated in the extensive study at the Menniger Foundation ((29)). We know from that study’s sophisticated methodology that this is not simply a halo effect but that it reflects a true independence between various aspects of mental health (A table of intercorrelations is available from the author upon request.).
Unreliability of Symptomatic Assessment
The relationship between symptomatic and clinical aspects of mental health alluded to in the previous section may be examined by classifying a subject as symptomatically ill if he obtained a score representing more than minimal impairment on at least 1 of the symptom variables in table 3. Then one can correlate this measure of illness with clinical illness as defined by a score representing more than minimal illness on the HSR scale. The degree of correlation between the two measures was relatively small for the 2 groups (=.46 for the former patients and .49 for the control subjects) ((30)).
However, separate examination of the degree of illness determined for the former patients and controls reveals an apparent bias in the results of the symptomatic assessment. Among the former patients, almost the same proportion was found to be symptomatically and clinically ill (69% versus 76%). However, a much higher proportion of the controls was found to be symptomatically than clinically ill (35% versus 15%). This difference between the 2 groups was just short of significance despite the small sample sizes (p=.052). Thus we add further evidence to the findings of Dohrenwend and associates ((31) ) and Masterson ((32)) that symptomatic assessment of controls leads to over-diagnosis of mental illness (Robins and Braroe ((33)) reported a similar finding, although they interpreted it differently) and that one must be very cautious in making conclusions based upon questionnaire-interview assessments of mental health. (TOP)
Discussion
Our principal finding is that most of the neurotic children had impaired mental health in adulthood, whereas most of the ordinary school children were not impaired. Is the different proportion of illness found in these 2 groups comparable to findings of previous studies and therefore of general significance? The only controlled study, that of Robins ((34)), suffers from a lack of direct clinical assessment. Even so, in that study there were significantly more healthy controls than former patients ((35), p. 137).
I examined in detail the reported findings of the various clinical follow-up studies ((36), (37), (38), (39), (40), (41), (42)) and found that case descriptions and descriptions of the frequency of various degrees of impairment permit some assessment of whether the degree of illness of those groups is generally comparable with ours. For instance, Levy ((43)) provided detailed case descriptions of the clinical follow-up picture of 19 children whose mothers were overprotective. Only 3 or 3 of these 19 former patients would appear to be well enough to have been rated healthy or only minimally ill on HSR. In all, I feel that the findings of all of these studies are quite compatible with ours and demonstrate substantial impairment when account is taken of differing methodology.
It is more difficult to find clinical studies of subjects who are comparable to our control group. We cannot compare our findings with those of the large-scale epidemiological studies for the reasons discussed earlier. I know of only one clinical study of a normal sample in which the levels of illness can be compared with those of our subjects. In that study ((44)) the low rates of illness for heads of households are quite comparable to those found in our control group. Therefore, such studies as we are able to find support our most important conclusion: children who come to a psychiatric clinic because of neurotic difficulties or developmental disturbances have an unfavorable prognosis for mental health in adulthood. This group of children is not identical to the large proportion of children who develop transient symptoms in the course of development, particularly during the oedipal period ((45), (46), (47)). For most of these children, psychiatric help is not sought.
We cannot determine directly the cause-and-effect relationship between referral for neurotic symptoms in childhood and adult mental health. But it is reasonable to assume that those children who cannot find a more adaptive way to resolve conflicts than the formation of such troublesome symptoms may be demonstrating an impaired capacity for neutralization or an impairment in ego strength that will lead to continuing unhealthy development ((48), p.235).
We cannot say on the basis of our sample whether the unfavorable prognosis applies to all groups of neurotic children. However, we may anticipate the findings to be reported in a later paper by saying that generally, it was not possible on the basis of the clinical picture in childhood to differentiate those neurotic children who would have good outcomes from the others. It may eventually be established that certain types of neurotic difficulties do not usually result in adult impairment, but there is no evidence from this study to support such a comforting conclusion.
The relationship between outcome and treatment received will also be the subject of a later report. It will suffice here to say that no patient received adequate treatment by psychoanalytic standards, If the treatment received resulted in some improvement for some of these children, then without intervention the former patients would have been, if anything, sicker. Thus our findings make necessary the conclusion that these children need effective treatment. What remains to be established is the validity of psychoanalytic clinicians’ impressions that sufficiently careful and intensive treatment in childhood frequently leads to good outcome in adulthood.
One methodological point deserves emphasis: the diagnostic approach to mental health is of somewhat limited utility and there is good reason to emphasize a quantitative assessment of degree of illness, which can be described as a dimensional approach to psychiatric disorder ((49)). Many areas of medicine have required just such grading of cases as the Health-Sickness Rating Scale provides (for instance, in the outcome of different grades of cervical cancers) before significant clarifications about prognosis can be made. Thus, although the clinical grading of psychiatric cases may not permit us to predict whether a child will develop a character disorder, a specific neurosis, or personality disorder, it does permit us to predict with some accuracy the later degree of illness. (TOP)
Conclusion
This study has provided evidence in support of the following points.
- Children with neurotic difficulties sufficient to bring them to professional attention have a much worse prognosis for adult mental health than normal control subjects. Therefore if any extensive psychotherapeutic technique such as child analysis can be shown to alter his prognosis, it should be used.
- Depending on the population involved, estimation of the degree of psychiatric disturbance through questionnaire-type interviews administered by non-professionals can lead to overestimation of the degree of illness and to substantially incorrect conclusions. Clinical assessment appears to be the only currently available method to avoid this pitfall.
- Approaching psychiatric illness from the point of view of degree of disturbance offers promising opportunities to enlarge our understanding and predictive powers, which may be obscured by too exclusive an adherence to a nosological approach.
REFERENCES
- Levitt, EE: The results of psychotherapy with children: an evaluation. J. Consult. Psychol. 2: 189-196, 1957.
- Freud A: Normality and pathology in Childhood. New York, International University Press, 1965
- Sundby HS (ed): Prognosis in Child Psychiatry. Baltimore, Williams & Wilkins Co, 1966
- Robins L: Deviant Children Grown Up. Baltimore, Williams & Wilkins Co, 1966
- Srole, L, Langner TS, Michael ST, et al: Mental Health in the Metropolis: The Midtown Manhattan Study, vol 1. New York, McGraw-Hill Book Co, 1962
- Leighton D, Harding JS, Macklin DB, et al: The Character of Danger. New York, Basic Books, 1963
- Dohrenwend B, Egri G, Mendelsohn F: Psychiatric disorders in general populations: a study of the problem of critical judgment. Am J Psychiatry 127: 1304-1312, 1971
- Morris DP, Soroker E, Burruss G: Follow-up studies of shy, withdrawn children. Evaluation of later adjustment. Am J Orthopsychiatry 24: 743-754, 1954
- Robins L, O’Neal P: Clinical features of hysteria in children, with a note on prognosis. A two- to seventee-year follow-up study of 41 patients. Nerv Child 10: 246-271, 1953
- Levy DM: Maternal Overprotection. New York, Columbia University Press, 1947
- Lebovitz PS: Feminine behavior in boys: aspects of its outcome. Am J Psychiatry 128: 1283-1289, 1972
- Apley J: The child with recurrent abdominal pain. Pediatr Clin North Am 14: 63-72, 1967
- Coolidge J, Brodie RD, Feeney B: A ten-year follow-up study of 66 school-phobic children. Am J Orthopsychiatry 34: 675-684, 1964
- Coolidge J, Brodie RD, Feeney B: A ten-year follow-up study of 66 school-phobic children. Am J Orthopsychiatry 34: 675-684, 1964
- Lessing E, Schilling F: Relationships between treatment selection variables and treatment outcome in a child guidance clinic. J Am Acad Child Psychiatry 5: 313-346, 1966
- Katz M, Cole J, Lowery H: Studies of the diagnostic process: the influence of symptom perception, past experience, and ethnic background on diagnostic decisions. Am J Psychiatry 125: 937-947, 1969
- Beck AT, Ward CH, mendelson M, et al: Reliability of psychiatric diagnosis: 2. A study of consistency of clinical judgments and ratings. Am J Psychiatry 119: 351-357, 1962
- Luborsky L: Clinicians’ judgments of mental health: a proposed scale. Arch Gen Psychiatry 7: 407-417, 1962
- Luborsky L, Bachrach H: factors influencing clinicians’ judgments of mental health. Arch Gen psychiatry 31: 292-299, 1974
- Endicott J, Spitzer R: Current and past Psychopathology Scales, Arch Gen Psychiatry 27: 678-687, 1972
- Walsdron S, Shrier DK, Stone B, et al: School phobia and other childhood neuroses: a systematic study of the children and their families. Am J Psychiatry 132: 802-808, 1975
- Group for the Advancement of Psychiatry: Psychopathological Disorders in Childhood: Theoretical Considerations and a Proposed Classification. Report 62. New York, GAP, 1966
- Robins L: Deviant Children Grown Up. Baltimore, Williams & Wilkins Co, 1966
- Levitt EE: On locating closed clinic cases for follow-up studies. Ment Hyg 42: 89-93, 1958
- Spitzer R, Endicott J: DIAGNO II: further developments in a computer program for psychiatric diagnosis. Am J Psychiatry 125(Jan Suppl): 12-21, 1969
- Coolidge J, Brodie RD, Feeney B: A ten-year follow-up study of 66 school-phobic children. Am J Orthopsychiatry 34: 675-684, 1964
- Fenichel O: The Psychoanalytic Theory of Neurosis. New York, WW Norton & Co, 1945
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 2nd ed. Washington, DC, APA, 1968
- Kernberg O, Burstein E, Coyne L, et al: Psychotherapy and Psychoanalysis: final report of the Menninger Foundation’s Psychotherapy Research Project. Bull Menninger Clin 36:1-275, 1972
- Spitzer R. Cohen J, Fleiss J, et al: Quantification of agreement in psychiatric diagnosis. Arch Gen Psychiatry 17:83-87, 1967
- Dohrenwend B, Egri G, Mendelsohn F: Psychiatric disorders in general populations: a study of the problem of critical judgment. Am J Psychiatry 127: 1304-1312, 1971
- Masterson JF: The Psychiatric Dilemma of Adolescence. Boston, Little, Brown and Co, 1967
- Robins L, Braroe N: The lay interviewer in psychiatric research. J Nerv Ment Dis 138:70-78, 1964
- Robins L: Deviant Children Grown Up. Baltimore, Williams & Wilkins Co, 1966
- Robins L: Deviant Children Grown Up. Baltimore, Williams & Wilkins Co, 1966
- Dohrenwend B, Egri G, Mendelsohn F: Psychiatric disorders in general populations: a study of the problem of critical judgment. Am J Psychiatry 127: 1304-1312, 1971
- Morris DP, Soroker E, Burruss G: Follow-up studies of shy, withdrawn children. Evaluation of later adjustment. Am J Orthopsychiatry 24: 743-754, 1954
- Robins L, O’Neal P: Clinical features of hysteria in children, with a note on prognosis. A two- to seventee-year follow-up study of 41 patients. Nerv Child 10: 246-271, 1953
- Levy DM: Maternal Overprotection. New York, Columbia University Press, 1947
- Lebovitz PS: Feminine behavior in boys: aspects of its outcome. Am J Psychiatry 128: 1283-1289, 1972
- Apley J: The child with recurrent abdominal pain. Pediatr Clin North Am 14: 63-72, 1967
- Coolidge J, Brodie RD, Feeney B: A ten-year follow-up study of 66 school-phobic children. Am J Orthopsychiatry 34: 675-684, 1964
- Levy DM: Maternal Overprotection. New York, Columbia University Press, 1947
- Dohrenwend B, Egri G, Mendelsohn F: Psychiatric disorders in general populations: a study of the problem of critical judgment. Am J Psychiatry 127: 1304-1312, 1971
- Freud A: Normality and pathology in Childhood. New York, International University Press, 1965
- Macfarlane J, Allen J, Honzik M: A Developmental Study of the Behavior Problems of Normal Children Between 21 Months and 14 Years. Berkeley, University of California Press, 1954
- Murphy L: The Widening World of Childhood. New York, Basic Books, 1962
- Hartmann H: Notes on the theory of sublimation (1955), in Essays on Ego Psychology. New York, International Universities Press, 1964, pp 215-240
- Strauss J: Diagnostic models and the nature of psychiatric disorders. Arch Gen Psychiatry 29:445-449, 1973